Each person is affected by disasters in different ways. However, the reasons for these disparities stem from factors that can and should be addressed pre-disaster. The public health field is implementing measures to address at-risk communities and to help mitigate public health threats, which increase in magnitude during disasters. The equitable efforts of five cities are shared in this article.
In the past few years, the public health field has moved to account for the conditions in which people are born, grow, live, work, and age that positively or negatively influence health. These social determinants are affected significantly by unequitable systemic policies, which are then experienced disproportionally by individuals and populations. For example, low-income communities and communities of color in the United States bear a disproportionate burden of disease in part due to access to preventative healthcare.
Framework for Disaster Health Resilience
This burden can only be fully explained by examining the environment and systems that these communities (and individuals) interface with daily. The social determinants framework has broadened the focus of disease management to include societal issues that affect health outcomes including: housing, food security, education, and systemic policies. This change has pushed public health to consider the true causes of disease and to look more fully at the communities that are most burdened by them, providing a health equity lens through which to consider health disparities and healthcare.
Similarly, a health equity lens should also be applied to healthcare preparedness and response policies in communities to contend with the disparities so they are not exacerbated during disasters. The incorporation of health equity into preparedness policies would acknowledge that systemic policies result in disproportionate access to public health services and healthcare, as well as disparities in health outcomes. This acknowledgment would foster improved emergency planning that accounts for and works toward addressing inequities. This shift is critical to emergency preparedness and response because these groups are also more vulnerable to the negative impacts of emergencies, especially natural disasters.
Low-income and predominantly minority communities are typically underresourced, have an overrepresentation of vulnerabilities to disease, and include large populations of individuals without consistent access to healthcare. Many of these communities are found in urban (or hyper-urban) regions, as well as the Gulf Coast and rural areas – regions prone to natural disasters and other threats. These communities are less able to cope with natural hazards due to continuous stressors and gaps in community resilience, which often result in disasters. Gaps in community preparedness and resilience are revealed during a disaster, exacerbating poor health outcomes that were already present. Disasters that disrupt public health and healthcare operations are happening more frequently, necessitating preparedness policies and practices that account for health inequities and build resilience.
Best Practices Across the Country
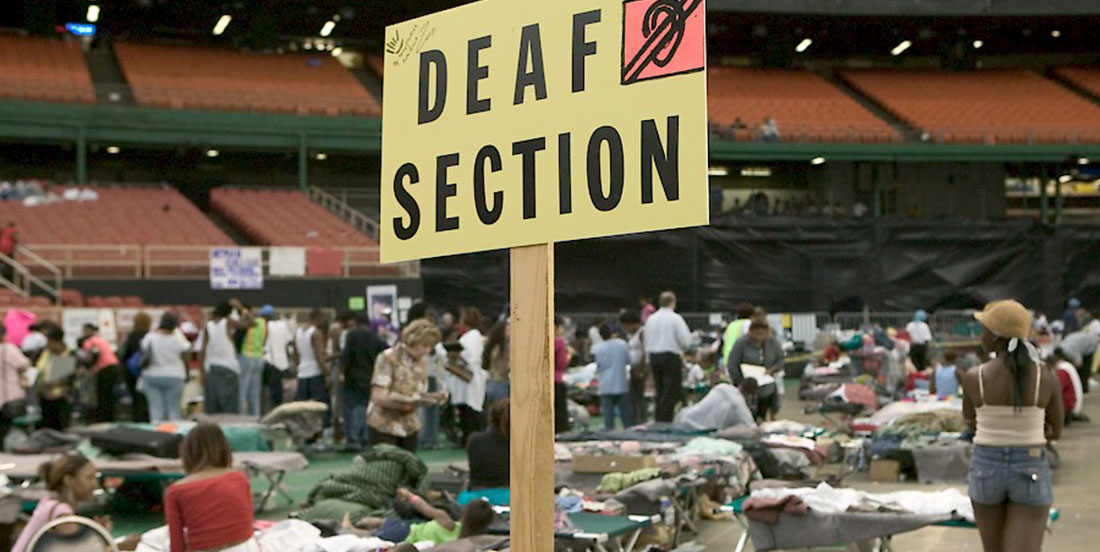
Finding ways to build and bridge relationships and improve resilience at the community level will require dedication to building trust and capacity by giving “the most to the least.” Community resilience can be promoted by prioritizing resources and preparedness efforts to communities with high need and vulnerability. Several cities are beginning to integrate equity-minded practices into their community resilience planning. Seattle-King County’s Department of Public Health is one such example, with focused inclusion efforts to remove systemic barriers for a wide range of groups and ensure that the entire community is better equipped to prepare for and respond to disasters. Its team has made a concerted effort to go into communities to engage populations, especially vulnerable populations, to hear their concerns and work to resolve the challenges faced by these groups. The population segments identified by Seattle-King County as being disproportionately at risk during a disaster are people who are: blind; clients of the criminal justice system; chemically dependent; children; deaf, deaf-blind, hard of hearing; developmentally disabled; homeless and shelter dependent; immigrant communities; impoverished; limited English or non-English proficient; medically dependent, medically compromised; mentally ill; physically disabled; seniors; and undocumented persons. By connecting with these groups in an equitable manner, Seattle-King County has fostered resilience by creating materials and resources specifically to assist these groups with emergency preparedness and resilience.
Other cities have taken similar measures to link their resilience work with health equity:
- Boston, Massachusetts, has created a chief resilience officer position to advance racial equity as a cornerstone of its work to improve community resilience.
- New York City has a health equity expert at the deputy commissioner level also directing its health equity work to eliminate health disparities.
- Baltimore, Maryland, is working through its Sustainability Commission and mayor’s office to create resilience hubs placed in communities to lead local preparedness efforts and serve as a primary conduit to emergency management and public health.
- In 2016, Austin, Texas, followed and created a chief equity officer position to help the city identify and resolve disparities in programs and policies.
There is still a need for more widespread consideration of the inequities disproportionately experienced by communities in disasters. Only in doing so will these communities have true resilience during disasters.

Nicolette Louissaint
Nicolette Louissaint, Ph.D., is the interim executive director at Healthcare Ready. Previously, she served as a foreign affairs officer at the U.S. Department of State in the Bureau of Economic and Business Affairs as the lead officer for health intellectual property and trade issues. During the height of the Ebola Epidemic of 2014, she served as the senior advisor to Ambassadors Nancy J. Powell and Steven A. Browning, the State Department’s special coordinators for Ebola. She holds degrees in Chemical Engineering and Biological Sciences from Carnegie Mellon University, as well as a Ph.D. in Pharmacology and Molecular Sciences from Johns Hopkins University School of Medicine.
- Nicolette Louissainthttps://domesticpreparedness.com/author/nicolette-louissaint
- Nicolette Louissainthttps://domesticpreparedness.com/author/nicolette-louissaint